Expedited Review of a Prior Authorization Request
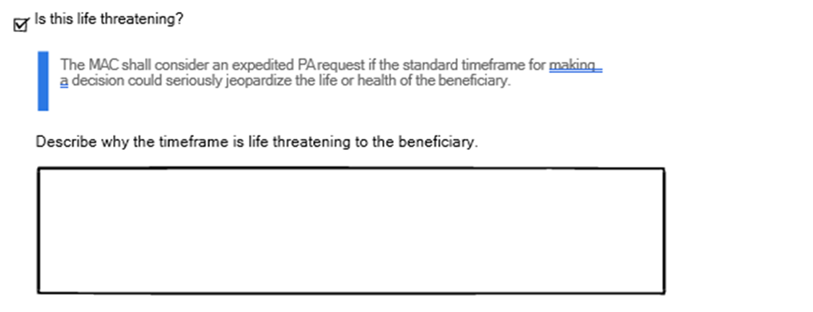
The requester can submit an expedited review of the prior authorization request (PAR) if it is determined that a delay could seriously jeopardize the beneficiary’s life, health, or ability to regain maximum function. The requester will be notified regarding the acceptance of the PAR for expedited review or if it will convert the request to the standard PA review process.
The affirmative or non-affirmative decision will be rendered within the CMS-prescribed expedited review timeframe of two business days for requests that are deemed valid for expedited review and provide the decision to the provider via telephone, fax, electronic portal, or other “real-time” communication within the requisite timeframe.
Expedited review is for a life-threatening situation, it should not be requested to get a faster determination in a non-life-threatening situation.
When requesting an expedited review, the provider must include an explanation why this procedure needs to be performed urgently.
Fax Form Submission
eServices Submission
Things to Remember When Submitting an Expedited PAR
- The request form must be fully completed
- An explanation of why the PAR is expedited must be included
- Expediting is for urgency and not because the procedure has already been scheduled
Resources: Prior Authorization (PA) Program for Certain Hospital Outpatient Department (OPD) Services Operational Guide (PDF).